Scientists Envision a Universal Coronavirus Vaccine
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Dr. Deborah Fuller, a professor of microbiology at the Washington University School of Medicine, in her lab.
With several companies progressing through Phase III clinical trials, the much-awaited coronavirus vaccines may finally become reality within a few months.
But some scientists question whether these vaccines will produce a strong and long-lasting immunity, especially if they aren't efficient at mobilizing T-cells, the body's defense soldiers.
"When I look at those vaccines there are pitfalls in every one of them," says Deborah Fuller, professor of microbiology at the Washington University School of Medicine. "Some may induce only transient antibodies, some may not be very good at inducing T-cell responses, and others may not immunize the elderly very well."
Generally, vaccines work by introducing an antigen into the body—either a dead or attenuated pathogen that can't replicate, or parts of the pathogen or its proteins, which the body will recognize as foreign. The pathogens or its parts are usually discovered by cells that chew up the intruders and present them to the immune system fighters, B- and T-cells—like a trespasser's mug shot to the police. In response, B-cells make antibodies to neutralize the virus, and a specialized "crew" called memory B-cells will remember the antigen. Meanwhile, an army of various T-cells attacks the pathogens as well as the cells these pathogens already infected. Special helper T-cells help stimulate B-cells to secrete antibodies and activate cytotoxic T-cells that release chemicals called inflammatory cytokines that kill pathogens and cells they infected.
"Each of these components of the immune system are important and orchestrated to talk to each other," says professor Larry Corey, who studies vaccines and infectious disease at Fred Hutch, a non-profit scientific research organization. "They optimize the assault of the human immune system on the complexity of the viral, bacterial, fungal and parasitic infections that live on our planet, to which we get exposed."
Despite their variety, coronaviruses share certain common proteins and other structural elements, Fuller explains, which the immune system can be trained to identify.
The current frontrunner vaccines aim to train our body to generate a sufficient amount of antibodies to neutralize the virus by shutting off its spike proteins before it enters our cells and begins to replicate. But a truly robust vaccine should also engender a strong response from T-cells, Fuller believes.
"Everyone focuses on the antibodies which block the virus, but it's not always 100 percent effective," she explains. "For example, if there are not enough titers or the antibody starts to wane, and the virus does get into the cells, the cells will become infected. At that point, the body needs to mount a robust T-cytotoxic response. The T-cells should find and recognize cells infected with the virus and eliminate these cells, and the virus with them."
Some of the frontrunner vaccine makers including Moderna, AstraZeneca and CanSino reported that they observed T-cell responses in their trials. Another company, BioNTech, based in Germany, also reported that their vaccine produced T-cell responses.
Fuller and her team are working on their own version of a coronavirus vaccine. In their recent study, the team managed to trigger a strong antibody and T-cell response in mice and primates. Moreover, the aging animals also produced a robust response, which would be important for the human elderly population.
But Fuller's team wants to engage T-cells further. She wants to try training T-cells to recognize not only SARV-CoV-2, but a range of different coronaviruses. Wild hosts, such as bats, carry many different types of coronaviruses, which may spill over onto humans, just like SARS, MERS and SARV-CoV-2 have. There are also four coronaviruses already endemic to humans. Cryptically named 229E, NL63, OC43, and HKU1, they were identified in the 1960s. And while they cause common colds and aren't considered particularly dangerous, the next coronavirus that jumps species may prove deadlier than the previous ones.
Despite their variety, coronaviruses share certain common proteins and other structural elements, Fuller explains, which the immune system can be trained to identify. "T-cells can recognize these shared sequences across multiple different types of coronaviruses," she explains, "so we have this vision for a universal coronavirus vaccine."
Paul Offit at Children's Hospitals in Philadelphia, who specializes in infectious diseases and vaccines, thinks it's a far shot at the moment. "I don't see that as something that is likely to happen, certainly not very soon," he says, adding that a universal flu vaccine has been tried for decades but is not available yet. We still don't know how the current frontrunner vaccines will perform. And until we know how efficient they are, wearing masks and keeping social distance are still important, he notes.
Corey says that while the universal coronavirus vaccine is not impossible, it is certainly not an easy feat. "It is a reasonably scientific hypothesis," he says, but one big challenge is that there are still many unknown coronaviruses so anticipating their structural elements is difficult. The structure of new viruses, particularly the recombinant ones that leap from wild hosts and carry bits and pieces of animal and human genetic material, can be hard to predict. "So whether you can make a vaccine that has universal T-cells to every coronavirus is also difficult to predict," Corey says. But, he adds, "I'm not being negative. I'm just saying that it's a formidable task."
Fuller is certainly up to the task and thinks it's worth the effort. "T-cells can cross-recognize different viruses within the same family," she says, so increasing their abilities to home in on a broader range of coronaviruses would help prevent future pandemics. "If that works, you're just going to take one [vaccine] and you'll have lifetime immunity," she says. "Not just against this coronavirus, but any future pandemic by a coronavirus."
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
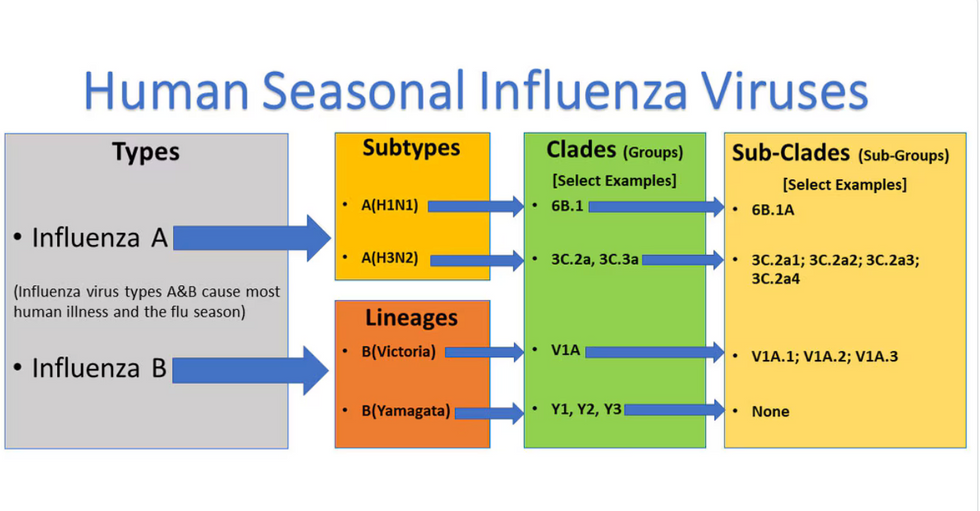
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

